Lesson 1Urine studies and interpretation: urinalysis, urine sediment microscopy, urine electrolytes, fractional excretion of sodium and ureaHere we cover getting and reading urine tests in sudden kidney injury on long-term disease, like urine analysis, looking at sediment under microscope, urine salts, and excretion rates, to tell apart causes before kidney, in kidney, or after kidney.
Standard urinalysis and dipstick findingsSediment microscopy and key castsUrine sodium and osmolality patternsFENa, FEUrea, and their limitationsIntegrating urine data with clinical contextLesson 2Acute complications requiring urgent action: hyperkalemia, severe acidosis, pulmonary edema, uremic manifestationsThis covers sudden problems in sudden kidney injury on long-term disease needing quick action, like high potassium, bad acid buildup, lung water, and waste buildup signs, focusing on steadying them and when to start emergency dialysis.
Emergency management of hyperkalemiaTreatment of severe metabolic acidosisRecognition and therapy of pulmonary edemaIdentifying uremic symptoms and signsDialysis triggers in acute complicationsLesson 3Definitions and staging of AKI and CKD, KDIGO criteria and integrationWe review what counts as sudden and long-term kidney injury, stages using KDIGO rules, mixing acute and chronic signs, and how stages guide outlook, watch closeness, and when to call specialists.
KDIGO AKI diagnostic criteriaKDIGO AKI staging and prognosisCKD definition, staging, and GFR categoriesIntegrating AKI on CKD classificationsImplications for follow-up and counselingLesson 4Pathophysiology of acute on chronic kidney injury: hemodynamic, intrinsic, and postrenal causesThis explores why sudden injury hits long-term weak kidneys, splitting flow issues, kidney itself problems, blockages after, and linking to patient signs, tests, and aimed fixes.
Hemodynamic causes and renal perfusionIntrinsic tubular and glomerular injuryPostrenal obstruction mechanismsNeurohormonal activation in CKD and AKIPathophysiology–guided treatment choicesLesson 5Identification and management of reversible precipitants: sepsis, nephrotoxins, volume depletion or overload, obstructionWe look at spotting and treating fixable triggers of sudden injury in long-term disease, like blood infection, kidney poisons, low or too much fluid, blockages, stressing quick fixes to stop more harm.
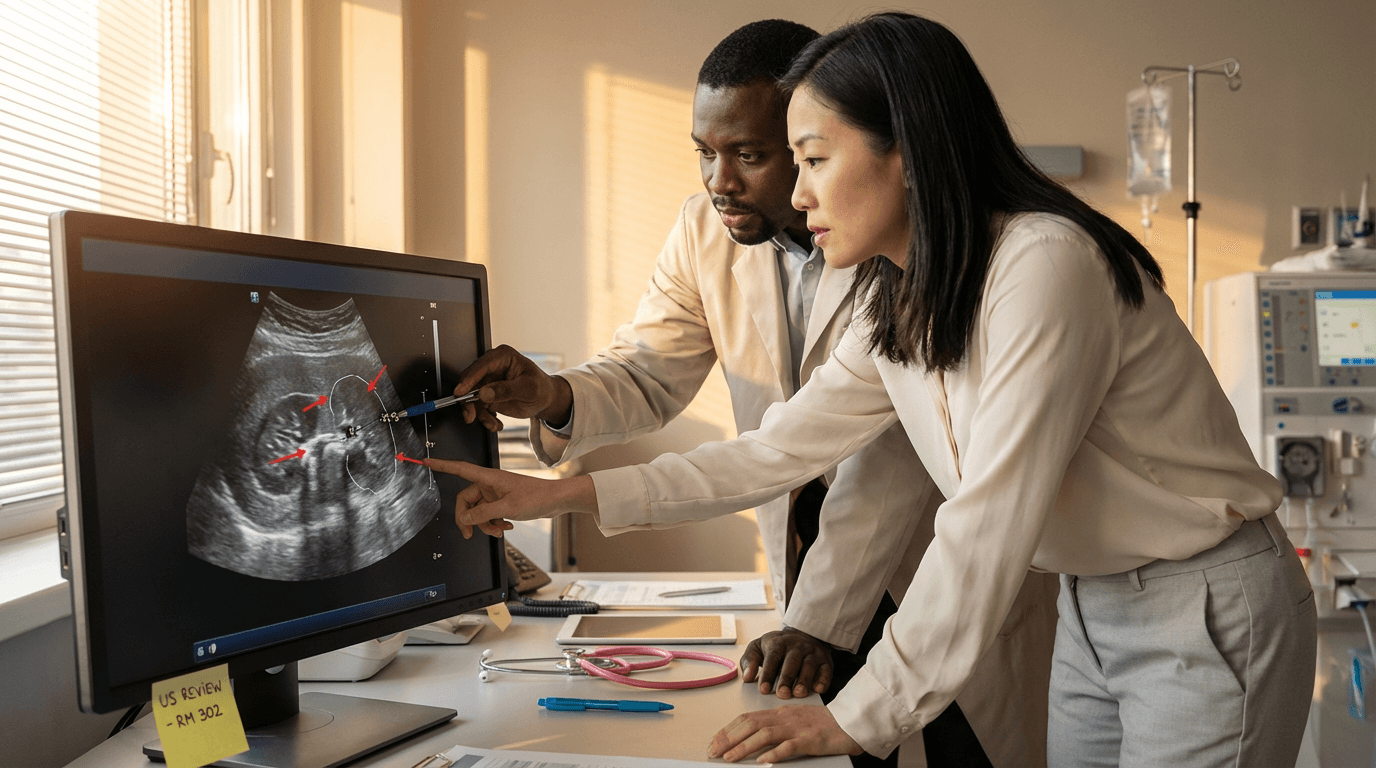
Recognizing sepsis and hemodynamic instabilityIdentifying and stopping nephrotoxic medicationsAssessing hypovolemia and fluid responsivenessManaging volume overload and decongestionDetecting and relieving urinary tract obstructionLesson 6Imaging indications and interpretation: renal ultrasound for obstruction, bladder scan, point-of-care ultrasound for volume statusThis explains when and how to use scans in sudden injury on long-term disease, like kidney ultrasound for blocks, bladder checks for hold-up, quick ultrasound for fluid levels, heart work, lung water.
Indications for renal ultrasoundRecognizing hydronephrosis and obstructionBladder scan for retention and retention riskPOCUS for IVC and volume assessmentLung and cardiac POCUS in AKI on CKDLesson 7Key laboratory interpretation: creatinine kinetics, BUN/creatinine ratio, electrolytes, acid-base analysis, lactateFocus on reading main lab results in sudden injury on long-term disease, like creatinine changes over time, BUN to creatinine ratio, salts, acid-base, lactate, to split new from old issues and guide quick steps.
Creatinine trends and baseline estimationUsing BUN/creatinine ratio in contextElectrolyte patterns in AKI on CKDAcid–base analysis and anion gap useLactate, perfusion, and tissue hypoxiaLesson 8Decision-making for renal replacement therapy in AKI: indications, timing, modality selection (intermittent hemodialysis vs CRRT vs SLED)This covers choices for dialysis in sudden injury on long-term disease, signs needed, timing talks, picking between short dialysis, continuous, or slow low, based on blood flow, tools, care aims.
Absolute and relative indications for RRTEarly versus delayed initiation strategiesChoosing intermittent HD versus CRRTWhen to use SLED and hybrid approachesAnticoagulation and access considerationsLesson 9Interdisciplinary communication with ICU, ED, primary teams and nursing for urgent AKI careStresses good talk between ICU, emergency, main teams, nurses in urgent kidney care, shared thinking, clear jobs, rise triggers, standard handovers for better safety and results.
Essential data to share during handoffClarifying roles and responsibilitiesEscalation criteria and rapid responseCommunicating dialysis urgency and plansDocumentation and closed-loop communicationLesson 10Initial rapid bedside assessment: history, focused exam, volume status, hemodynamicsOutlines bedside steps for sudden injury on long-term disease, mixing patient story, aimed exam, fluid check, blood flow check to spot life dangers and likely causes fast.
Key history elements in AKI on CKDFocused exam for perfusion and congestionBedside tools for volume status assessmentBlood pressure, MAP, and perfusion targetsRisk stratification for deterioration and ICU