Lesson 1Urine studies and interpretation: urinalysis, urine sediment microscopy, urine electrolytes, fractional excretion of sodium and ureaThis part explains how to collect and read urine tests in AKI on CKD, covering urinalysis, sediment under microscope, urine electrolytes, and fractional excretion measures to tell apart prerenal, intrinsic, and postrenal causes for better diagnosis.
Standard urinalysis and dipstick findingsSediment microscopy and key castsUrine sodium and osmolality patternsFENa, FEUrea, and their limitationsIntegrating urine data with clinical contextLesson 2Acute complications requiring urgent action: hyperkalemia, severe acidosis, pulmonary edema, uremic manifestationsThis part deals with urgent problems from AKI on CKD like high potassium, bad acidosis, lung water buildup, and uremic signs, focusing on quick stabilisation and when to start emergency dialysis.
Emergency management of hyperkalemiaTreatment of severe metabolic acidosisRecognition and therapy of pulmonary edemaIdentifying uremic symptoms and signsDialysis triggers in acute complicationsLesson 3Definitions and staging of AKI and CKD, KDIGO criteria and integrationThis part goes over definitions and stages for AKI and CKD using KDIGO guidelines, how to combine acute and chronic changes, and how stages guide outlook, monitoring level, and when to call specialists.
KDIGO AKI diagnostic criteriaKDIGO AKI staging and prognosisCKD definition, staging, and GFR categoriesIntegrating AKI on CKD classificationsImplications for follow-up and counselingLesson 4Pathophysiology of acute on chronic kidney injury: hemodynamic, intrinsic, and postrenal causesThis part looks at how acute on chronic kidney injury happens, separating blood flow issues, kidney tissue damage, and blockage after the kidney, linking to clinic signs, tests, and targeted treatments.
Hemodynamic causes and renal perfusionIntrinsic tubular and glomerular injuryPostrenal obstruction mechanismsNeurohormonal activation in CKD and AKIPathophysiology–guided treatment choicesLesson 5Identification and management of reversible precipitants: sepsis, nephrotoxins, volume depletion or overload, obstructionThis part covers spotting and treating fixable AKI triggers in CKD like infections, kidney poisons, low or high fluid volume, and blockages, with focus on quick fixes to stop more kidney harm.
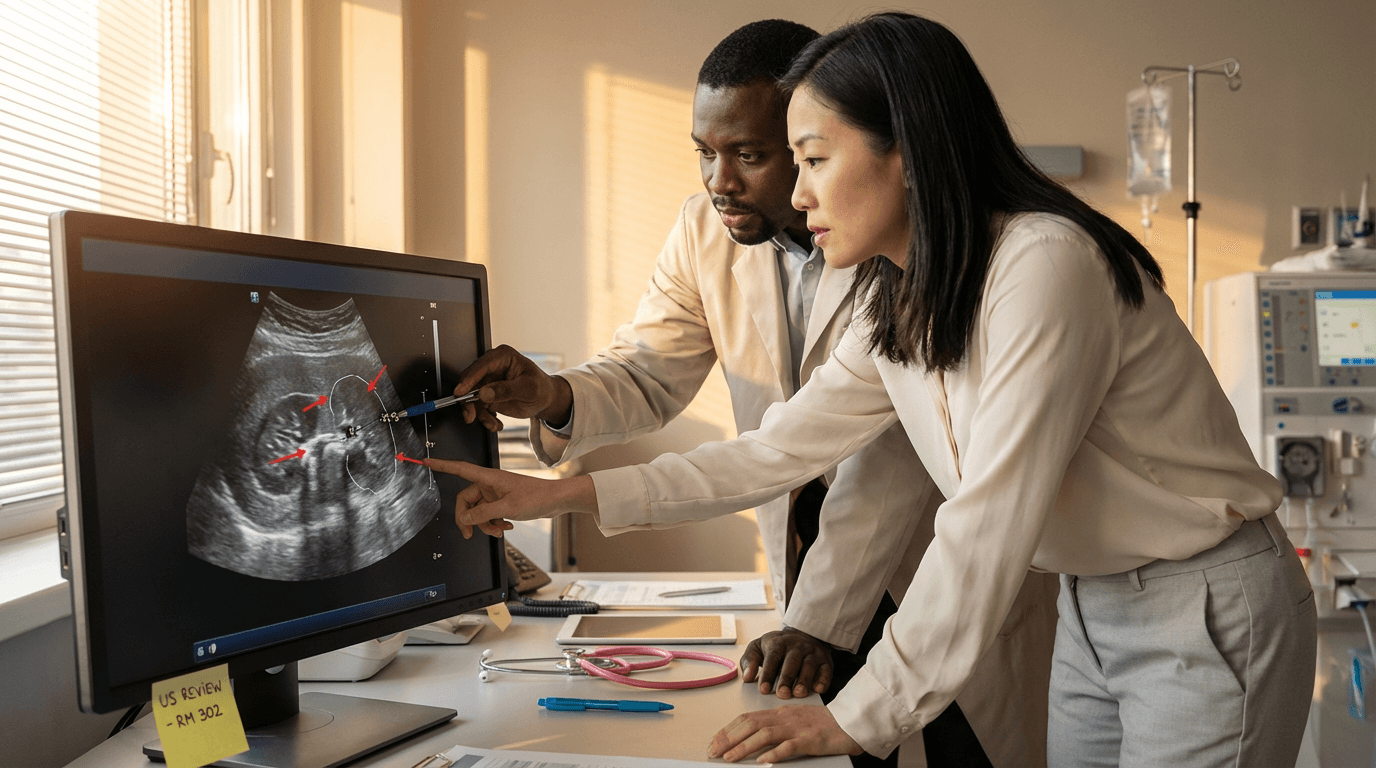
Recognizing sepsis and hemodynamic instabilityIdentifying and stopping nephrotoxic medicationsAssessing hypovolemia and fluid responsivenessManaging volume overload and decongestionDetecting and relieving urinary tract obstructionLesson 6Imaging indications and interpretation: renal ultrasound for obstruction, bladder scan, point-of-care ultrasound for volume statusThis part teaches when and how to use scans in AKI on CKD, like kidney ultrasound for blockages, bladder checks for holding urine, and quick bedside ultrasound for fluid levels, heart work, and lung fluid.
Indications for renal ultrasoundRecognizing hydronephrosis and obstructionBladder scan for retention and retention riskPOCUS for IVC and volume assessmentLung and cardiac POCUS in AKI on CKDLesson 7Key laboratory interpretation: creatinine kinetics, BUN/creatinine ratio, electrolytes, acid-base analysis, lactateThis part stresses reading main lab results in AKI on CKD, like creatinine changes over time, BUN to creatinine ratio, salts, acid-base balance, and lactate, to separate new from old issues and guide urgent care.
Creatinine trends and baseline estimationUsing BUN/creatinine ratio in contextElectrolyte patterns in AKI on CKDAcid–base analysis and anion gap useLactate, perfusion, and tissue hypoxiaLesson 8Decision-making for renal replacement therapy in AKI: indications, timing, modality selection (intermittent hemodialysis vs CRRT vs SLED)This part covers choices for kidney replacement in AKI on CKD, including usual triggers, timing talks, and picking between short dialysis, continuous replacement, or slow low dialysis based on blood stability, available tools, and care aims.
Absolute and relative indications for RRTEarly versus delayed initiation strategiesChoosing intermittent HD versus CRRTWhen to use SLED and hybrid approachesAnticoagulation and access considerationsLesson 9Interdisciplinary communication with ICU, ED, primary teams and nursing for urgent AKI careThis part highlights good teamwork talk among ICU, emergency, main teams, and nurses in urgent AKI care, focusing on shared thinking, clear job sharing, escalation signs, and standard handovers for better safety and results.
Essential data to share during handoffClarifying roles and responsibilitiesEscalation criteria and rapid responseCommunicating dialysis urgency and plansDocumentation and closed-loop communicationLesson 10Initial rapid bedside assessment: history, focused exam, volume status, hemodynamicsThis part lays out a clear bedside check for AKI on CKD, mixing patient history, targeted exam, fluid status check, and blood flow review to quickly spot life dangers and likely AKI causes.
Key history elements in AKI on CKDFocused exam for perfusion and congestionBedside tools for volume status assessmentBlood pressure, MAP, and perfusion targetsRisk stratification for deterioration and ICU